3 Factors Surrounding Medicaid & Managed Care Organizations
In partnership with states nationwide, risk-based Managed Care Organizations (MCOs) coordinate essential healthcare services for Medicaid enrollees living with intellectual and developmental disabilities (IDD). Over the last decade, COVID-19 and other global and national events have greatly influenced the utilization of risk-based MCOs. Direct Care Innovations has adapted to these changes and continues to support MCOs with our direct care business management software. We invite you to explore three factors surrounding current Medicaid enrollment and risk-based managed care.
1. Influence of COVID-19 on Medicaid Enrollment
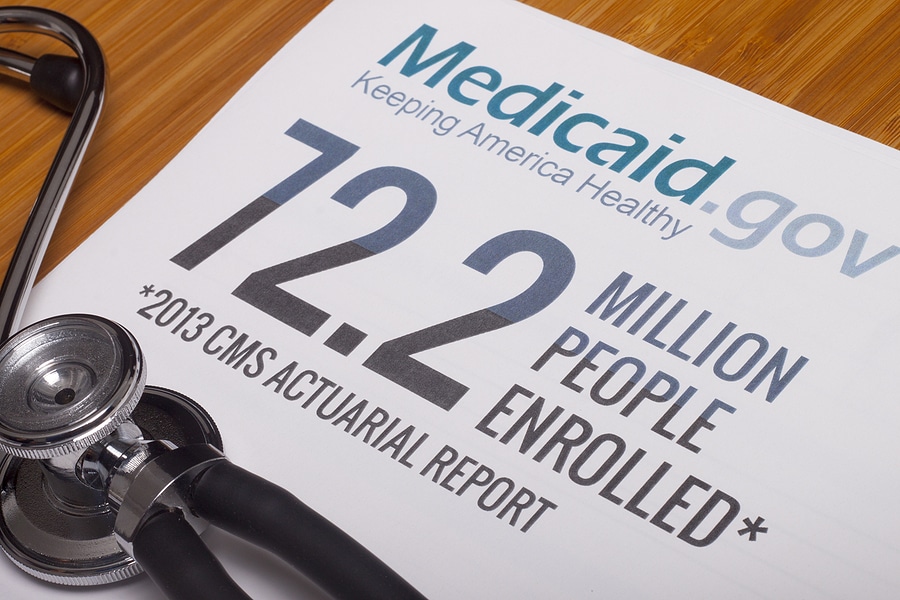
During the COVID-19 public health emergency, federal policy prohibited states from unenrolling beneficiaries or conducting annual renewals or redeterminations. This resulted in a substantial growth in Medicaid enrollment. In December 2019, there were 71 million enrollees compared to an all-time high of 94.5 million in April 2023, when the Medicaid “unwinding process” began. Eight months later, in December 2023, Medicaid enrollees had decreased by almost 10%. Various strategies were available to help eligible individuals keep their Medicaid coverage while states processed renewals. These included allowing time for enrollees to update their contact information, permitting MCOs to help enrollees complete required paperwork, and extending automatic Medicaid re-enrollment from 60 to 120 days.
2. Projected Capitation Rates & Risk Mitigation Strategies
Rather than paying specific fees for services, states make upfront fixed payments, or capitation payments, to Medicaid MCOs. Capitation payments are calculated on a per month per enrollee basis and cover contractually available Medicaid services and other related costs. Federal regulations require capitation rate payments to be actuarially sound — monthly payments are projected based on appropriate costs, contract terms, managed care plan administration, and specific populations being covered.
As pandemic-related enrollment increased, the Centers for Medicare & Medicaid Services permitted states to modify Medicaid/MCO contracts by implementing risk-based strategies. About two-thirds of MCO states implemented COVID-related “risk corridors,” an agreement between states and health plans to share profit or losses. More than 75% of these states recouped capitation payments made between 2020 and 2022. Average loss ratios were also lower in 2021, hinting toward increased profitability.
3. Strategies to Identify & Address Health Gaps
Understanding that social, behavioral, and healthcare needs can influence the well-being of Medicaid enrollees, states are implementing strategies to identify and define social determinants of health, improve health equity, and reduce health discrepancies. Before 2024, CMS took steps to decrease gaps and improve care services by providing waivers for the availability of certain tools and resources and issuing guidelines on using “in lieu of” services. In 2023, most MCO states implemented at least one strategy to address social determinants of health. Over half of MCO states require that Medicaid enrollees be screened for behavioral health and social needs, receive referrals to social services, and collaborate with community organizations and agencies.
Simplify Your System with DCI
Our mission is to reinvent direct care administration to create a sustainable future. When you partner with Direct Care Innovations, your Managed Care Organization will experience increased compliance, fewer billing errors, seamless EVV and data aggregation solutions, improved care management, and more. Request a sales demo or call (480) 295-3307 today.
Hinton, Elizabeth and Raphael, Jada, “10 Things to Know About Medicaid Managed Care,” KFF, May 01, 2024.

